In the on-going debate of which drug addiction treatment is more effective, naltrexone is showing more potential than buprenorphine, according to a latest study by researchers from Columbia University.
The results of the study will have a profound impact on the $35-billion drug addiction treatment market as this could influence which treatment method gets the bigger slice of the pie.
Maria Sullivan, MD, PhD, of College of Physicians and Surgeons of Columbia University and lead researcher of the study, said that an outpatient detoxication regimen using naltrexone was more effective for transitioning adults with opioid dependence to extended-release naltrexone than a regimen using buprenorphine.
Sullivan said, “An extended-release injectable form of naltrexone has FDA approval for relapse prevention following opioid detoxification. However, a substantial barrier to its effective implementation is the need to detoxify patients from opioids before naltrexone is initiated.”
About Naltrexone
Naltrexone is a popular medication used to block the effects of opioids. The oral form is sold under the brand name Revia, which is manufactured by Barr Laboratories, a subsidiary of Teva Pharmaceuticals (NYSE: TEVA), an Israeli-based pharmaceutical giant with $19.7 billion in revenues in 2015. A once-monthly extended-release injectable formulation is marketed under the trade name Vivitrol, which is manufactured by Alkermes PLC, (Nasdaq: ALKS), an $8-billion pharmaceutical company.
Brady Granier, president, CEO and director of BioCorRx, Inc. (OTC-Pink: BICX), a California company developing sustained release naltrexone products under its subsidiary BioCorRx Pharmaceuticals, stated “naltrexone has multiple uses and is an old, but fascinating medication. It’s effective for both alcoholism and opioid addiction and is worthy of becoming the gold standard for relapse prevention.”
Researchers Say Naltrexone with Initial Dose of Buprenorphine Can Increase Patient Acceptability
The researchers at Columbia University said in their report, “The study results support the feasibility of ascending low doses of oral naltrexone, in combination with an initial dose of buprenorphine and standing nonopioid ancillary medications, as an outpatient regimen for opioid detoxification and [extended-release naltrexone] induction. By circumventing the need for a protracted period of abstinence and mitigating the severity of withdrawal symptoms experienced during detoxification, this strategy has the potential to considerably increase patient acceptability of, and access to, antagonist therapy.”
The researchers conducted the study amongst 150 individuals with opioid dependence who were selected randomly to assess the efficacy of an approach for transitioning adults with opioid dependence to extended-release injection naltrexone while preventing relapse. The participants were assigned to receive naltrexone-assisted detoxification or buprenorphine-assisted detoxification followed by an injection of extended-release naltrexone.
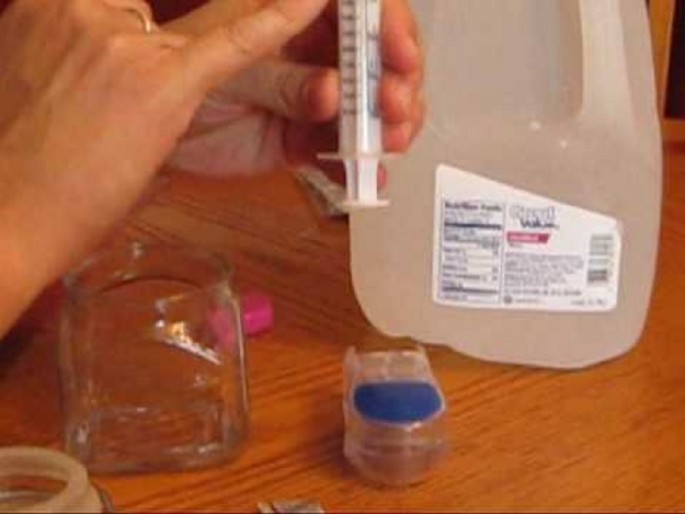
Naltrexone-assisted detoxification included one day of buprenorphine followed by increasing doses of oral naltrexone, clonidine and other adjunctive medications for seven days. Buprenorphine-assisted detoxification included a seven-day buprenorphine taper followed by a seven-day delay before administration of extended-release naltrexone.
Participants who received naltrexone-assisted detoxification were significantly more likely to receive extended-release naltrexone (56.1 percent vs. 32.7 percent) and receive a second injection at week 5 (50 percent vs. 26.9 percent), compared with the buprenorphine-assisted group.
These findings remained consistent when adjusting for primary type of opioid use, route of opioid administration and morphine equivalents at baseline.
Patients Treated With Buprenorphine More Likely To Disengage From Treatment
A separate study published in the Journal of Substance Abuse Treatment showed that black, or Hispanic patients with opioid dependency who are treated with buprenorphine are more likely to discontinue the treatment program. The same observation was made amongst patients with opioid dependency who have hepatitis C.
Another study was conducted by the Boston University School of Medicine (BUSM) and (BUSPH) Public Health by examining patients treated at the Boston Medical Center’s (BMC) Office Based Addiction Treatment (OBAT) program between 2002 and 2014 to better understand why certain groups disengage from buprenorphine treatment.
Researchers have found that many individuals who participate in OBAT with buprenorphine discontinue treatment less than one year after the initiation. It added that older patients, females, and co-morbid psychiatric diagnosed patients show higher treatment retention after one year, but black, Hispanic, unemployed, and those with hepatitis C have decreased chances of retaining treatment after one year.
Brady added, “I’m encouraged by the advances in detoxification products and protocols. There are many new treatments on the horizon that should allow for a more efficient and tolerable transition from opioids to sustained released naltrexone products by those suffering.
Currently, BioCorRx is in the early stage of developing a new injectable naltrexone product called BICX101 under its subsidiary BioCorRx Pharmaceuticals. BioCorRx said that it plans to offer BICX101 at a lower price than the leading Vivitrol brand and expects BICX101 to be less painful when administered due to an anticipated smaller needle size and less injection volume.